
Weakening of intervertebral discs or other spinal disorders that complicate or limit movement indicate the development of a serious disease - osteochondrosis. It can occur in anyone and is not associated with age. The spine is a supporting element of the skeleton, therefore its changes affect the quality of life and the condition of many organic systems. Therefore, it is necessary to know the causes, signs of osteochondrosis, as well as treatment methods in order to notice disorders in time and prevent the development of pathology.
What is osteochondrosis
Osteochondrosis is a complex of degenerative diseases of the human spine, which are manifested by dystrophic changes in the cartilage of this system.The disease can occur in any joint, but it develops much more frequently in the intervertebral discs.
The main sign that indicates the development of the disease is pain in the back, neck and lower back. In the future, pain may be felt in the shoulders, arms and upper thighs. In the absence of treatment, atrophy of muscle tissue begins, disturbance of the sensitivity and activity of internal organs, which leads to an incurable condition.
ICD-10 Code
The World Health Organization developed the ICD-10 (International Classification of Diseases, 10th revision). Its essence is as follows: each disease has its own specific code, consisting of numbers and letters. The doctor, seeing such a code in front of him, knows exactly what disease we are talking about and what treatment should be prescribed to save the patient from this problem.
According to ICD-10, osteochondrosis has the code M42 and belongs to the class "Diseases of the musculoskeletal system and connective tissue" (group "Dorsopathies", subgroup "Deforming dorsopathies").
Causes of development and risk factors
There are many reasons for the occurrence of osteochondrosis. They all depend on which part of the spine the disease develops - cervical, thoracic or lumbar. There are several main reasons for the development of the disease:
- Hereditary predisposition. Congenital anomalies contribute to the development of diseases of the musculoskeletal system;
- Hormonal imbalance. Disturbance of the endocrine system, being overweight or underweight negatively affects the musculoskeletal system;
- Age-related changes in the body. As a result of this, muscle, bone and cartilaginous tissues are destroyed, intervertebral discs wear out with age;
- Spine injuries and bruises. Many people spend a lot of time in one position, for example sitting at a desk, while others do the same type of physical work. All of this causes damage to the bone and ligament apparatus of the spine, as well as injuries to the intervertebral discs;
- Degenerative changes in muscle tissue. These processes appear due to excessive tension of individual muscle groups, which most often leads to thoracic osteochondrosis.
- Sedentary lifestyle. Muscle atrophy occurs, which causes circulatory disorders and inadequate formation of the bone skeleton.
Most people are inattentive to their diet, eating foods that are not at all healthy. As a result, nutritional deficiency occurs, which negatively affects the integrity of the intervertebral cartilage, its mobility and elasticity.
There are several risk factors for developing this disease:
- hypothermia;
- flat foot;
- complications after infectious diseases;
- overweight;
- sedentary lifestyle;
- Spine injuries.
When intervertebral discs and cartilaginous tissue are damaged, it is important to determine the cause of the disease and initiate appropriate treatment.
Types and symptoms
Depending on the localization of the pathological process, several types of osteochondrosis are distinguished.
Osteochondrosis of the cervical spine
It manifests as pain in the neck, back of the head and between the shoulder blades. During sleep, neck mobility may be limited. Often with cervical osteochondrosis, numbness in the fingers occurs. Dizziness and tinnitus are also observed. Varieties of cervical osteochondrosis differ in clinical manifestations:
- neck pain– accompanied by neck pain and difficulty moving; the pain may spread to the shoulder area and the space between the shoulder blades; Tingling and burning sensations can often be observed in the hands and fingers;
- cervicocranialgia– accompanied by pain from the neck to the parietal and occipital parts of the head, shoulder girdle; muscular tension is characteristic, a feeling of petrification is created; headaches, nausea, tinnitus, imbalance are observed;
- cervicobrachialgia– characterized by sharp, aching, pulling and throbbing pains; turning and tilting the head can cause an attack of sharp pain and physical tension in the affected area, pain occurs in the arms and fingers, leading to weakness of the upper limbs;
- discogenic root injury– characterized by paroxysmal pain in the shoulders, forearms and fingers, accompanied by numbness and a feeling of cold; symptoms intensify when coughing, sneezing or turning the head suddenly; it may worsen at night, leading to insomnia.
Osteochondrosis of the thoracic spine

This is a rather rare form. In terms of symptoms, thoracic osteochondrosis is similar to other diseases and therefore requires differential diagnosis.As a result of the immobility of the thoracic vertebrae in this area, severe pain during movement is not observed.The pain syndrome spreads to the sternum and under the shoulder blade. Thoracic osteochondrosis can cause disruptions in the functioning of internal organs. The main clinical manifestations of thoracic osteochondrosis are:
- Thoracalgia or intercostal neuralgia– is irritation or compression of the intercostal nerves by muscles and tissues, which is accompanied by pain in the chest when bending, bending and turning the body, under the ribs, in front of the chest, pain when inhaling, exhaling; pain may radiate to the shoulder and between the shoulder blades;
- pain syndrome, in which the pain is of an acute nature; pain can be felt inside the chest, abdomen; worsens with movement, coughing, sneezing, laughing; sensitivity disturbances are observed.
Thoracalgia (chest pain) is one of the most serious symptoms a person can experience. Sometimes even a doctor cannot immediately determine the cause of chest pain and find out whether this symptom is a sign of a threat to the patient's life.
Osteochondrosis of the lumbosacral region
The main reason for such changes is a lack of nutrients and heavy loads. The metabolism slows down, and as a result, the discs do not have time to renew themselves, their structure and properties are disturbed. There are several types of lumbar osteochondrosis:
- low back pain (acute low back pain)– acute pain in the lumbar spine that occurs when lifting weights, performing physical activities or bending over; characterized by sharp pain on the right or left in the lower back; also distinguish low back pain with sciatica, when the pain spreads to the buttocks and legs;
- radicular vascular syndrome (radiculoischemia)occurs when the radiculomedullary artery is damaged and is accompanied by paralysis of the extensors and flexors of the gluteal muscle group, the foot hangs loosely, there is no movement.
Osteochondrosis of the spine with radicular-vascular syndrome is a very dangerous pathology, which is expressed in sharp pain, since CSS is often a consequence of some disease.
Development stages
The stages of osteochondrosis are characterized as follows:
- The initial phase begins with the loss of fluid reserves in the nucleus pulposus of the intervertebral discs. As a resultthe physiological position of the disc and the structure of the nucleus pulposus are disturbed.
- Further development of the disease (first degree) is due to a decrease in disc height.Muscles and ligaments become overloaded and lose their ability to function normally.At this stage, vertebral displacement may appear.
- The second degree is characterized by changes in bone tissue.Forms of arthrosis, subluxations occur.
- The third degree is determined by the fact thatbone growths (osteophytes) form in the spine,which lead to damage to the nerve roots.
The development of osteochondrosis should not be neglected, since with each subsequent stage the course of treatment and rehabilitation increases. Complications that develop during the illness can lead to undesirable consequences.
What is the difference between radiculitis and osteoarthritis?
The symptoms of osteochondrosis and radiculitis are very similar, but the main difference between them is that in the first case they occur only in the later stages, while radiculitis is characterized by the early manifestation of severe symptoms.Furthermore, in radiculitis, pressure on the paravertebral muscles and even tilting the head cause severe pain., resembling an electric shock, which does not happen in osteochondrosis.
Comparing osteochondrosis and arthrosis, it is important to note that in the second disease all elements of the joint are affected, resulting in crunching and limited mobility. Osteochondrosis, in turn, is characterized by the destruction of intervertebral discs with the formation of hernial protrusions.
Differential diagnostic methods are used to determine the disease. This is a comprehensive approach that requires effort and time.
Diagnosis
If osteochondrosis is suspected, the doctor prescribes a comprehensive diagnosis, which consists of the following studies.

Neurological examination
It is performed by a neurologist. This exam includes checking reflexes, muscle strength and the extent of pain in other parts of the body.Neurological examination is very important for osteochondrosis, because this disease affects the functioning of nerve endings and the spinal cord.
Spine myelography
Allows you to see how cerebrospinal fluid spreads within the spinal membranes. This helps to identify pathologies of the spine, diseases of the nerve roots and spinal cord. Under local anesthesia, a special dye is injected into the region of the spinal cord and nerves. An X-ray machine provides a complete picture of the spine, especially the bones. This method allows you to identify any deviations.
Computed tomography (CT)
These are photos of one or two segments of the spine. Using this procedure, you can see an image of the bone tissue of a particular region of the spine. The doctor interprets the resulting image and, if a narrowing of the space between the vertebrae is visible, this indicates that the patient has osteochondrosis.
Nuclear magnetic resonance (NMR)
MRI uses strong magnetic fields, as well as radio waves, to create images of the human body from individual scans.With this method, ligaments, tendons and bone structures are very well differentiated.
Magnetic resonance imaging (MRI)
It is an effective procedure because it has a safe effect on the body - during the procedure, results are obtained through the use of a magnetic field and not radiation.
You cannot agree to the prescribed treatment without a comprehensive preliminary diagnosis. This can only lead to deterioration of health.
Treatment methods
Treatment of osteochondrosis involves many complex measures.Depending on the severity of the disease, a specific treatment strategy is selected.
Drug therapy
As a rule, the treatment of osteochondrosis begins with the use of a certain group of medications:
- analgesics and various pain relievers;
- medicines that relieve spasms;
- vitamins B and C;
- medicines that relieve inflammation;
- medicines that promote better blood circulation.
In addition to taking medications orally, patients are prescribed various nonsteroidal ointments and gels that can relieve pain and reduce swelling in problem areas.
Physiotherapy
In addition to drug therapy, various physiotherapeutic procedures are used. Thanks to this method, medications can be administered directly to the site of inflammation. Main types of physiotherapy:
- Electrophoresis– carrying out physiotherapy with electric fields modulated by currents. This allows medications to be introduced into the body. Helps relieve pain and muscle spasms;
- Magnetotherapy. This painless physiotherapy involves the positive effect of a magnetic field on the active cells of nerve and muscle fibers. As a result, the work of molecular structures is activated and the functional properties of blood vessels are improved;
- Ultrasound Therapy. Ultrasound are sound waves produced in a range that the human ear cannot perceive. Thanks to this, blood circulation in the affected areas improves, relieves spasms, eliminates pain and stops inflammatory processes;
- Vibration effect. With the help of mechanical vibrations, the affected area is affected;
- Balneotherapy. The essence of the method is the use of mineral water, which relaxes the muscles and has a beneficial effect on the musculoskeletal system. Use mineral water in the shower or bathtub.

Physiotherapy should be carried out during the period of weakening of symptoms, when there is no pain. In the acute phase of the disease, the doctor selects a set of procedures that can eliminate the pain syndrome. With adequate physical treatment, the patient stops feeling pain, the spine becomes more mobile, which indicates recovery.
Traditional methods
Treatment of osteochondrosis may include the use of folk recipes, the effectiveness of which depends on the individual characteristics of the body. Here are some of them:
- You will need 300 g of radish juice, 200 g of honey and 100 g of vodka. Mix all the ingredients and lubricate the affected areas 2 times a day.
- You will need 1 tbsp. I. rye flour, 100 g of butter, 1 tbsp. I. vinegar and 1 egg. Mix all the ingredients and leave for two days. Rub into affected areas.
- Grate the raw potatoes and mix with a little honey. Apply the prepared pulp to the sore spot for 2 hours.
Traditional treatment methods cannot act as independent therapy.To obtain a visible and lasting result, you must combine medicinal, conservative and folk methods.
Traction

Spinal traction is often used for osteochondrosis. With the help of traction, muscle spasm is relieved, displacement of the vertebrae and deformation of the spine are eliminated. The procedure is performed in a hospital. There are dry and underwater methods of spinal traction.
Dry traction is carried out under the influence of the weight of the patient, who lies on an inclined plane.To increase traction force, the doctor may use additional weights. With underwater traction, the healing effect is enhanced by the effect of warm water on the body.
Under the influence of water, the distance between the vertebrae increases, vascular spasms in the affected area are eliminated and blood supply improves.
Surgery
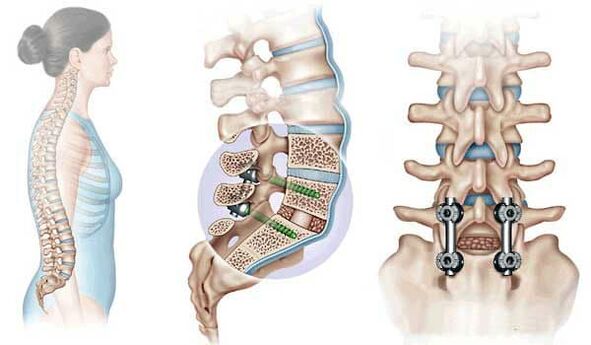
Surgical treatment of osteochondrosis is carried out in cases where there are serious complications.Such complications include: intervertebral disc herniation, vertebral displacement and significant decrease in the lumen of the spinal canal.
In this case, several types of operations are performed. These include operations to protect displaced vertebrae with metal plates, insert artificial intervertebral joint implants, or remove individual bone growths.
Physiotherapy
Physiotherapy for osteochondrosis is one of the most important aspects of treatment. As a result, blood circulation is gradually restored, the vertebrae return to their normal position and the spine is significantly strengthened.
In the initial stages of the disease, it consists of gymnastics.In cases where gymnastics does not bring positive results, the doctor selects an individual set of exercises for the patient, combined with other physiotherapy procedures.
Complications
The disease can cause the following complications:
- inflammatory diseases of the nerve roots (radiculitis, radiculopathy);
- intervertebral hernia;
- vegetative-vascular dystonia;
- various neurological complications;
- severe headaches, migraines;
- limb atrophy;
- spinal canal stenosis;
- spondyloarthrosis (proliferation of the edges of the articular surface as a result of deforming arthrosis);
- stroke in the spinal cord.
If drug therapy does not bring positive results, surgical treatment is prescribed. The slightest delay and failure to start treatment on time can lead to disability, as the spine will lose its properties and mobility.
If therapeutic therapy is not started in a timely manner, complications such as malfunctions in the organs of the reproductive and urinary systems may occur.
Prevention
Treating osteochondrosis is quite difficult. Therefore, every effort must be made to prevent the disease from arising in the body. To prevent the occurrence of osteochondrosis, it is necessary to constantly carry out preventive measures:
- Rightorganize a workplace;
- when working you needtake short breaksdoing light gymnastics;
- watch your posture;
- dailygait should be easy, without constriction;
- choose the right and comfortable pillow, elastic mattress.The sleeping surface must be flatand elastic;
- The daily diet should contain a minimum of salty and sweet dishes and more foods enriched with calcium. Vitamins C, E, B must be present. They will strengthen the cartilaginous tissue and make it elastic.
- active lifestyle.
- prophylacticmassage.
- medicinalfitness.
Preventive measures are also the main requirements during the rehabilitation period. Following these simple rules allows you to avoid a relapse of the disease even after complete recovery.
conclusions
- Osteochondrosis is a degenerative disease of the human spine. Symptoms depend on the type of disease and the place of occurrence (cervical, thoracic, lumbosacral).
- Complications of the disease can not only disrupt the integrity of the spine, but also significantly affect the functioning of other organ systems.
- Osteochondrosis can only be cured comprehensively, combining medication, physiotherapy and therapeutic exercises.
- It's not complicatedPreventive measures will help protect your body from serious pathologies.



















